Infertility, Its cause and Treatment Biology Investigatory Project PDF Class 12

Abstract
Infertility is the inability of a person, animal or plant to reproduce by natural means. It is usually not the natural state of a healthy adult organism, except notably among certain eusocial species (mostly haplodiploid insects).
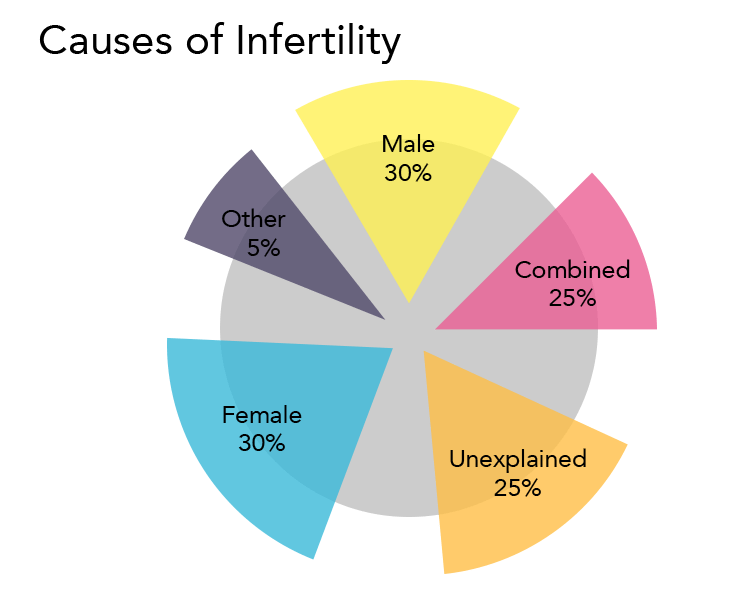
In humans, infertility may describe a woman who is unable to conceive as well as being unable to carry a pregnancy to full term. There are many biological and other causes of infertility, including some that medical intervention can treat. Infertility rates have increased by 4% since the 1980s, mostly from problems with fecundity due to an increase in age. About 40% of the issues involved with infertility are due to the man, another 40% due to the woman, and 20% result from complications with both partners.
Women who are fertile experience a natural period of fertility before and during ovulation, and they are naturally infertile during the rest of the menstrual cycle. Fertility awareness methods are used to discern when these changes occur by tracking changes in cervical mucus or basal body temperature
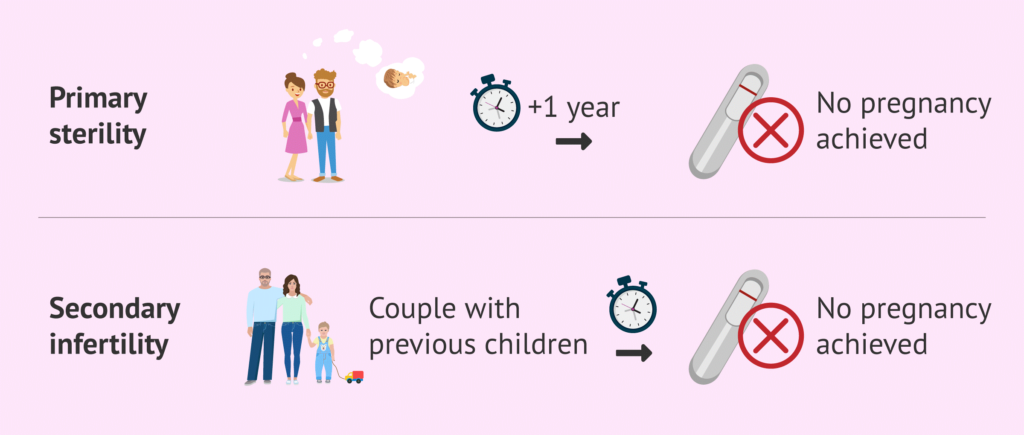
Infertility is “a disease of the reproductive system defined by the failure to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse (and there is no other reason, such as breastfeeding or postpartum amenorrhea). Primary infertility is infertility in a couple who have never had a child. Secondary infertility is failure to conceive following a previous pregnancy. Infertility may be caused by infection in the man or woman, but often there is no obvious underlying cause.
Theory
Researchers commonly base demographic studies on infertility prevalence on a five-year period. Practical measurement problems, however, exist for any definition, because it is difficult to measure continuous exposure to the risk of pregnancy over a period of years.
Primary Vs Secondary Infertility
Primary infertility is defined as the absence of a live birth for women who desire a child and have been in a union for at least five years, during which they have not used any contraceptives. The World Health Organization also adds that ‘women whose pregnancy spontaneously miscarries, or whose pregnancy results in a still born child, without ever having had a live birth would present with primarily infertility.
Secondary infertility is defined as the absence of a live birth for women who desire a child and have been in a union for at least five years since their last live birth, during which they did not use any contraceptives.
Thus, the distinguishing feature is whether or not the couple have ever had a pregnancy which led to a live birth.
Effect of Infertility
Psychological impact
The consequences of infertility are manifold and can include societal repercussions and personal suffering. Advances in assisted reproductive technologies, such as IVF, can offer hope to many couples where treatment is available, although barriers exist in terms of medical coverage and affordability. The medicalization of infertility has unwittingly led to a disregard for the emotional responses that couples experience, which include distress, loss of control, stigmatization, and a disruption in the developmental trajectory of adulthood.
Infertility may have profound psychological effects. Partners may become more anxious to conceive, increasing sexual dysfunction Marital discord often develops in infertile couples, especially when they are under pressure to make medical decisions. Women trying to conceive often have clinical depression rates similar to women who have heart disease or cancer. Even couples undertaking IVF face considerable stress.
The emotional losses created by infertility include the denial of motherhood as a rite of passage; the loss of one’s anticipated and imagined life; feeling a loss of control over one’s life; doubting one’s womanhood; changed and sometimes lost friendships; and, for many, the loss of one’s religious environment as a support system.
Emotional stress and marital difficulties are greater in couples where the infertility lies with the man.
Social impact
In many cultures, inability to conceive bears a stigma. In closed social groups, a degree of rejection (or a sense of being rejected by the couple) may cause considerable anxiety and disappointment. Some respond by actively avoiding the issue altogether; middle-class men are the most likely to respond in this way.
In an effort to end the shame and secrecy of infertility, Redbook in October 2011 launched a video campaign, The Truth About Trying, to start an open conversation about infertility, which strikes one in eight women in the United States.
In a survey of couples having difficulty conceiving, conducted by the pharmaceutical company Merck, 61 percent of respondents hid their infertility from family and friends. Nearly half didn’t even tell their mothers. The message of those speaking out: It’s not always easy to get pregnant, and there’s no shame in that.
There are legal ramifications as well. Infertility has begun to gain more exposure to legal domains. An estimated 4 million workers in the U.S. used the Family and Medical Leave Act (FMLA) in 2004 to care for a child, parent or spouse, or because of their own personal illness. Many treatments for infertility, including diagnostic tests, surgery and therapy for depression, can qualify one for FMLA leave. It has been suggested that infertility be classified as a form of disability.
Cause of Infertiltiy
Infertility can have various causes, affecting both men and women. Here are some common factors:
- Age:
As women age, their fertility decreases due to a decline in the quantity and quality of eggs. Similarly, aging can affect sperm quality and quantity in men. - Reproductive System Disorders:
Conditions such as polycystic ovary syndrome (PCOS), endometriosis, fibroids, and pelvic inflammatory disease (PID) can interfere with fertility in women. In men, conditions like varicocele (enlarged veins in the testes), sperm duct defects, and erectile dysfunction can affect fertility. - Hormonal Imbalances:
Hormonal disorders, such as thyroid problems or abnormal levels of reproductive hormones like estrogen, progesterone, testosterone, and follicle-stimulating hormone (FSH), can impact fertility in both men and women. - Lifestyle Factors:
Unhealthy lifestyle habits like smoking, excessive alcohol consumption, drug abuse, poor diet, obesity, and lack of exercise can negatively affect fertility. - Sexual Issues:
Problems with sexual function or intercourse, such as erectile dysfunction or painful intercourse, can contribute to infertility. - Environmental Factors:
Exposure to certain environmental toxins, chemicals, pesticides, and pollutants can impair fertility.
- Genetic Factors:
Inherited genetic conditions or chromosomal abnormalities can affect fertility in both men and women. - Medical Treatments:
Certain medical treatments such as chemotherapy, radiation therapy, and surgeries may affect reproductive organs and impair fertility. - Psychological Factors:
Stress, anxiety, and depression can affect hormone levels and interfere with ovulation and sperm production.
Female Infertility
The following causes of infertility may only be found in females. For a woman to conceive, certain things have to happen: intercourse must take place around the time when an egg is released from her ovary; the system that produces eggs has to be working at optimum levels; and her hormones must be balanced.
For women, problems with fertilisation arise mainly from either structural problem in the Fallopian tube or uterus or problems releasing eggs. Infertility may be caused by blockage of the Fallopian tube due to malformations, infections such as Chlamydia and/or scar tissue. For example, endometriosis can cause infertility with the growth of endometrial tissue in the Fallopian tubes and/or around the ovaries. Endometriosis is usually more common in women in their mid-twenties and older, especially when postponed childbirth has taken place.
Another major cause of infertility in women may be the inability to ovulate. Malformation of the eggs themselves may complicate conception. For example, polycystic ovarian syndrome is when the eggs only partially developed within the ovary and there is an excess of male hormones. Some women are infertile because their ovaries do not mature and release eggs. In this case synthetic FSH by injection or Clomid (Clomiphene citrate) via a pill can be given to stimulate follicles to mature in the ovaries. Other factors that can affect a woman’s chances of conceiving include being overweight or underweight, or her age as female fertility declines after the age of 30. Sometimes it can be a combination of factors, and sometimes a clear cause is never established.
- Common causes of infertility of females include:
- Ovulation Problems
- Tubal Blockage
- Pelvic Inflammatory disease caused by Infections like Tuberculosis
- Age-Related Factors
- Uterine Problems
- Previous Tubal Ligation
- Endometriosis
- Advanced Maternal Age
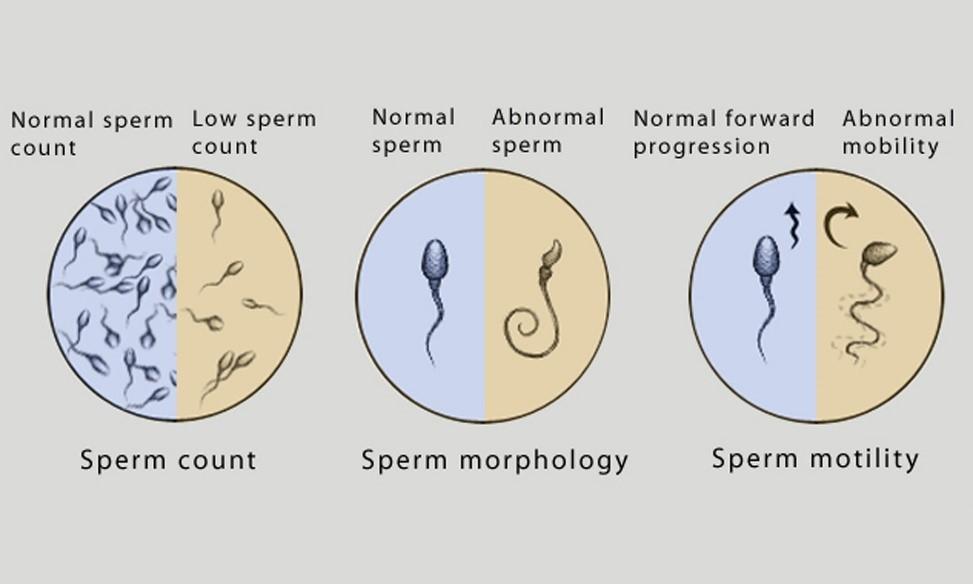
Male Infertility
The main cause of male infertility is low semen quality. In men who have the necessary reproductive organs to procreate, infertility can be caused by low sperm count due to endocrine problems, drugs, radiation, or infection. There may be testicular malformations, hormone imbalance, or blockage of the man’s duct system. Although many of these can be treated through surgery or hormonal substitutions, some may be indefinite. Infertility associated with viable, but immotile sperm may be caused by primary ciliary dyskinesia.
Combined infertility
In some cases, both the man and woman may be infertile or sub-fertile, and the couple’s infertility arises from the combination of these conditions. In other cases, the cause is suspected to be immunological or genetic; it may be that each partner is independently fertile but the couple cannot conceive together without assistance.
Unexplained infertility
In the US, up to 20% of infertile couples have unexplained infertility. In these cases abnormalities are likely to be present but not detected by current methods. Possible problems could be that the egg is not released at the optimum time for fertilization, which it may not enter the fallopian tube, sperm may not be able to reach the egg, fertilization may fail to occur, transport of the zygote may be disturbed, or implantation fails. It is increasingly recognized that egg quality is of critical importance and women of advanced maternal age have eggs of reduced capacity for normal and successful fertilization.
Treatment
Treatment depends on the cause of infertility, but may include counselling, fertility treatments, which include in vitro fertilization. According to ESHRE recommendations, couples with an estimated live birth rate of 40% or higher per year are encouraged to continue aiming for a spontaneous pregnancy. Treatment methods for infertility may be grouped as medical or complementary and alternative treatments. Some methods may be used in concert with other methods. Drugs used for both women and men include clomiphene citrate, Human Menopausal Gonadotropin (hMG), Follicle-Stimulating Hormone (FSH), Human Chorionic Gonadotropin (hCG), Gonadotropin-Releasing Hormone (GnRH) analogues, aromatase inhibitors, and metformin
Medical treatments
Medical treatment of infertility generally involves the use of fertility medication, medical device, surgery, or a combination of the following. If the sperm are of good quality and the mechanics of the woman’s reproductive structures are good (patent fallopian tubes, no adhesions or scarring), a course of ovarian stimulating medication maybe used. The physician or WHNP may also suggest using a conception cap cervical cap, which the patient uses at home by placing the sperm inside the cap and putting the conception device on the cervix, or Intrauterine Insemination (IUI), in which the doctor or WHNP introduces sperm into the uterus during ovulation, via a catheter. In these methods, fertilization occurs inside the body.
If conservative medical treatments fail to achieve a full-term pregnancy, the physician may suggest the patient undergo in Vitro Fertilization (IVF). IVF and related techniques (ICSI, ZIFT, and GIFT) are called Assisted Reproductive Technology (ART) techniques.
ART techniques generally start with stimulating the ovaries to increase egg production. After stimulation, the physician surgically extracts one or more eggs from the ovary, and unites them with sperm in a laboratory setting, with the intent of producing one or more embryos. Fertilization takes place outside the body, and the fertilized egg is reinserted into the woman’s reproductive tract, in a procedure called embryo transfer
Other medical techniques are e.g. tuboplasty, assisted hatching, and Preimplantation genetic diagnosis.
Ethical Issues
There are several ethical issues associated with infertility and its treatment.
- High-cost treatments are out of financial reach for some couples.
- Debate over whether health insurance companies (e.g. in the US) should be required to cover infertility treatment.
- Allocation of medical resources that could be used elsewhere.
- The legal status of embryos fertilized in vitro and not transferred in vivo. (See also Beginning of pregnancy controversy).
- IVF and other fertility treatments have resulted in an increase in multiple births, provoking ethical analysis because of the link between multiple pregnancies, premature birth, and a host of health problems.
- Religious leaders’ opinions on fertility treatments; for example, the Roman Catholic Church views infertility as a calling to adopt or to use natural treatments (medication, surgery, and/or cycle charting) and members must reject assisted reproductive technologies.
- Infertility caused by DNA defects on the Y chromosome is passed on from father to son. If natural selection is the primary error correction mechanism that prevents random mutations on the Y chromosome, then fertility treatments for men with abnormal sperm (in particular ICSI) only defer the underlying problem to the next male generation.
Many countries have special frameworks for dealing with the ethical and social issues around fertility treatment.
- One of the best known is the HFEA – The UK’s regulator for fertility treatment and embryo research. This was set up on 1 August 1991 following a detailed commission of enquiry led by Mary Warnock in the 1980s.
- A similar model to the HFEA has been adopted by the rest of the countries in the European Union. Each country has its own body or bodies responsible for the inspection and licencing of fertility treatment under the EU Tissues and Cells directive.
- Regulatory bodies are also found in Canada and in the state of Victoria in
- In India, The Assisted Reproductive Technology (Regulation) Act, 2021, was passed on December 20, 2021 by an act of Parliament to regulate the functioning of assisted reproductive technology (ART) clinics and ART banks in the country.
Conclusion
In conclusion, infertility presents a complex and multifaceted challenge affecting individuals, couples, and society at large. With increasing rates observed globally, understanding the causes, impacts, and treatment options for infertility is crucial for addressing this issue effectively.
The investigation into infertility has revealed a myriad of factors contributing to its occurrence, ranging from biological and genetic to environmental and lifestyle-related influences. Both men and women can experience infertility due to various reproductive system disorders, hormonal imbalances, genetic predispositions, and medical treatments. Psychological factors such as stress and anxiety further exacerbate the challenges faced by individuals and couples struggling with infertility.
The social and emotional impact of infertility cannot be overstated, as it often leads to feelings of distress, loss, and stigma within communities. Despite advancements in assisted reproductive technologies offering hope to many couples, barriers related to accessibility and affordability persist, underscoring the need for comprehensive support systems and awareness campaigns.
Ethical considerations surrounding infertility treatment, including the allocation of resources, legal status of embryos, and religious perspectives, further complicate the landscape of reproductive healthcare. However, regulatory frameworks and guidelines implemented in various countries aim to address these ethical dilemmas and ensure responsible practices within the field of assisted reproductive technology.
In light of these findings, efforts to destigmatize infertility, improve access to fertility treatments, and provide holistic support to affected individuals and couples are essential. By fostering open dialogue, raising awareness, and advocating for inclusive healthcare policies, we can work towards mitigating the social, emotional, and financial burdens associated with infertility, ultimately empowering individuals to pursue their reproductive aspirations with dignity and support.