Study of Cancer Biology Investigatory Project PDF Class 12

What is Cancer?
Cancer is characterized by the uncontrolled proliferation of abnormal cells anywhere in the body. These abnormal cells, also known as cancer cells, malignant cells, or tumour cells, can invade and disrupt normal body tissues. Cancers are often named after the tissue or organ where these abnormal cells originated, such as breast cancer, lung cancer, or colorectal cancer. Cancer is not exclusive to humans; animals and other living organisms can also develop cancer.
The diagram below illustrates the process of normal cell division and what happens when a cell is damaged or altered without undergoing repair. Typically, such damaged cells will die. However, if these damaged or unrepaired cells do not die, they can become cancer cells, leading to uncontrolled cell division and growth, forming a mass of cancer cells. Cancer cells can sometimes detach from the original mass, travel through the bloodstream or lymphatic system, and establish new growths in other parts of the body. This process is called metastatic spread or metastasis. For instance, if breast cancer cells spread to the bones, it results in metastatic breast cancer in the bones, which is distinct from “bone cancer,” where the cancer would have originated in the bone itself.
Types of Cancer
- Breast Cancer
Breast cancer develops in the cells of the breast, most commonly in the ducts or lobules. It is the most prevalent cancer among women worldwide, though men can also develop it. Risk factors include being female, advancing age, a family history of breast cancer, and genetic mutations like BRCA1 and BRCA2. Hormone replacement therapy and certain lifestyle factors, such as alcohol consumption and obesity, can also increase the risk.
Diagnosis typically involves a combination of self-exams, mammograms (X-ray of the breast), ultrasound, MRI, and biopsy where a sample of breast tissue is examined under a microscope.
- Lung Cancer
Lung cancer begins in the lungs and is strongly associated with smoking, although non-smokers can also develop the disease. The primary risk factor is smoking, but other factors include exposure to radon gas, asbestos, air pollution, and a family history of lung cancer. Those with a history of chronic lung disease may also be at higher risk.
Diagnosis is usually through imaging tests such as chest X-rays and CT scans, followed by a biopsy or sputum cytology, where mucus coughed up from the lungs is examined for cancer cells.
- Prostate Cancer
Prostate cancer develops in the prostate gland, which is responsible for producing seminal fluid in men. It is more common in older men, particularly those over 50, and is more frequently diagnosed in African American men. Risk factors include age, family history, and diet, particularly diets high in red meat and dairy products.
Diagnosis is often made using a combination of a digital rectal exam (DRE), prostate-specific antigen (PSA) blood test, and a biopsy, where prostate tissue is sampled and examined. - Colorectal Cancer
Colorectal cancer originates in the colon or rectum, often beginning as benign polyps that can turn cancerous over time. Risk factors include being over the age of 50, a diet high in red or processed meats, and a personal or family history of colorectal cancer or polyps. Inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis also increase the risk.
Diagnosis is commonly through screening methods like colonoscopy, where the inside of the colon is examined with a camera, and fecal occult blood tests (FOBT), which check for blood in the stool. Biopsies may also be taken during a colonoscopy. - Skin Cancer (including Melanoma)
Skin cancer, including melanoma and non-melanoma types, arises from the skin cells, often due to excessive exposure to ultraviolet (UV) radiation from the sun or tanning beds. Those with fair skin, a history of sunburns, or a family history of skin cancer are at greater risk. A large number of moles or atypical moles can also increase the likelihood of developing melanoma.
Diagnosis involves a visual examination of the skin, dermatoscopy (using a special magnifying tool to examine the skin), and a biopsy where suspicious skin lesions are removed and examined under a microscope. - Bladder Cancer
Bladder cancer begins in the cells lining the bladder and is often linked to smoking and exposure to certain industrial chemicals. Risk factors include smoking, which is the most significant risk factor, as well as occupational exposure to substances like arsenic and certain dyes. Chronic bladder inflammation or infections can also contribute to the risk.
Diagnosis is typically made through urine tests (to detect blood or abnormal cells), cystoscopy (where a camera is inserted into the bladder), and a biopsy of bladder tissue. Imaging tests like CT urograms or intravenous pyelograms may also be used. - Non-Hodgkin Lymphoma
Non-Hodgkin lymphoma is a cancer that starts in the lymphatic system, with many different subtypes affecting the lymph nodes and other lymphoid tissues. Risk factors include a weakened immune system, such as in individuals with HIV/AIDS or those who have undergone organ transplants. Certain viral infections, age, and autoimmune diseases also play a role in increasing risk.
Diagnosis often involves blood tests, imaging tests like CT scans or PET scans, and a biopsy of lymph node tissue. Bone marrow biopsies may also be performed to see if the cancer has spread. - Kidney Cancer
Kidney cancer, most commonly renal cell carcinoma, originates in the kidneys. Smoking is a significant risk factor, along with obesity, high blood pressure, and a family history of the disease. Those with a history of kidney disease or certain genetic conditions are also at higher risk.
Diagnosis is usually done through imaging tests such as ultrasound, CT scans, or MRI, often followed by a biopsy where a sample of kidney tissue is examined. Urine tests and blood tests may also be used to assess kidney function and detect abnormalities. - Endometrial (Uterine) Cancer
Endometrial cancer begins in the lining of the uterus and is often associated with hormonal imbalances. Risk factors include obesity, which can alter hormone levels, as well as the use of hormone replacement therapy, particularly estrogen without progesterone. Never having been pregnant and advancing age are additional risk factors.
Diagnosis often involves a pelvic exam, transvaginal ultrasound, and endometrial biopsy, where a sample of the uterine lining is taken and examined. Hysteroscopy may also be used to view the inside of the uterus. - Pancreatic Cancer
Pancreatic cancer develops in the tissues of the pancreas and is often detected at a late stage. The risk factors include smoking, obesity, a family history of pancreatic cancer, chronic pancreatitis, and diabetes. Individuals with certain genetic mutations are also at increased risk.
Diagnosis typically involves imaging tests such as CT scans, MRI, or endoscopic ultrasound (EUS). A biopsy, often performed during an EUS or through fine-needle aspiration, is used to confirm the diagnosis. Blood tests may also be used to look for specific tumour markers. - Leukaemia
Leukaemia is a cancer of the blood or bone marrow characterized by the uncontrolled proliferation of abnormal white blood cells. Risk factors include previous exposure to radiation or certain chemotherapy treatments, as well as genetic disorders like Down syndrome. Some types of leukaemia are more common in adults, while others primarily affect children.
Diagnosis is usually through blood tests that show abnormal levels of white blood cells, red blood cells, or platelets. Bone marrow biopsy is also a key diagnostic tool, where a sample of bone marrow is extracted and examined. - Thyroid Cancer
Thyroid cancer arises in the thyroid gland at the base of the neck, with a higher incidence in women. Risk factors include being female, exposure to radiation (especially during childhood), and a family history of thyroid cancer or other thyroid conditions. Certain genetic syndromes can also increase the likelihood of developing this cancer.
Diagnosis involves a combination of physical exams, blood tests to check thyroid function, ultrasound imaging, and a fine-needle aspiration biopsy, where a small sample of thyroid tissue is taken for examination.
Sign and Symptom
- Unexplained weight loss, often seen in cancers of the pancreas, stomach, or lungs, is a sudden and significant loss of weight without effort.
- Persistent fatigue that doesn’t improve with rest can signal various cancers, including leukaemia or those causing chronic illness.
- Unusual skin changes, such as new growths or changes in moles, can signal skin cancer or cancers that have spread to the skin.
- Changes in bowel or bladder habits, such as blood in stool or urine, can indicate cancers like colorectal or bladder cancer.
- A chronic cough or hoarseness that doesn’t resolve may suggest lung cancer or cancers affecting the throat.
- Unexplained bleeding or bruising, like blood in urine or stool, can be signs of cancers including bladder, kidney, or blood cancers.
- Lumps or thickening in areas such as the breast, testicles, or lymph nodes can indicate cancers like breast cancer or lymphoma.
- Difficulty swallowing or a feeling of food being stuck can be symptoms of cancers of the esophagus, throat, or stomach.
- Persistent indigestion, nausea, or discomfort after eating might signal cancers of the stomach or esophagus.
- Changes in the mouth, like white or red patches or sores that don’t heal, can be signs of oral cancer.
- Swollen lymph nodes, particularly in the neck, armpits, or groin, can indicate cancers such as lymphoma or leukaemia.
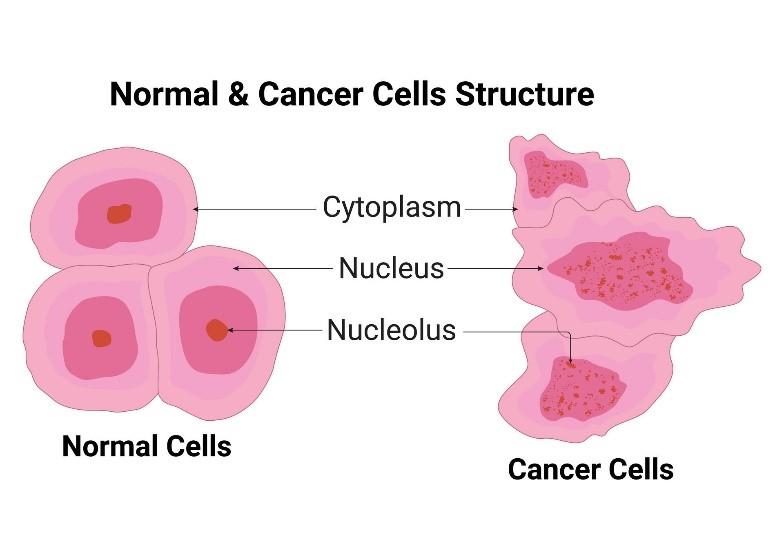
Difference between Normal Cells and Cancer Cells
Normal cells follow a typical cycle: They grow, divide and die. Cancer cells, on the other hand, don’t follow this cycle. Instead of dying, they multiply out of control and continue to reproduce other abnormal cells. These cells invade body parts, such as the breast, liver, lungs and pancreas.
Characteristics | Normal Cells | Cancer Cells |
Shape | Regular | Irregular |
Nucleus | Proportionate Size | Larger, Darker |
Growth | In Control, Systematic | Out of Control |
Maturation | Mature | Immature |
Communication | Communicates | Don’t Communicate |
Visibility | Visible to Immune Cells | Invisible to Immune Cells |
Blood Supply | Angiogenesis During Repair | Tumour Angiogenesis |
Oxygen | Requires Oxygens | Doesn’t Require Oxygen |
Glucose | Requires Some Glucose | Loves, Craves Glucose |
Energy Efficiency | Very High (95%) | Very Low (5%) |
Amount of ATP | 38 Units of ATP | 2 Units Of ATP |
Cell Environment | Alkaline | Acidic |
Nutrient Preference | Fat, Ketone, Glucose | Glucose |
Formation of Cancer Cells
Cancer cells form through a multi-step process known as carcinogenesis, which involves the transformation of normal cells into malignant ones. The process begins with the initiation stage, where genetic mutations occur within the DNA of a normal cell. These mutations can be caused by various factors, including exposure to carcinogens (such as those found in tobacco smoke or environmental pollutants), radiation (like ultraviolet rays from the sun or ionizing radiation from medical imaging), or inherited genetic mutations. Over time, these mutations accumulate, leading to changes in the cell’s behaviour and function. The affected cell may begin to grow and divide uncontrollably, bypassing the normal regulatory mechanisms that keep cell growth in check. As the process progresses, the mutated cell can acquire additional mutations, further enhancing its ability to proliferate and evade the immune system. This uncontrolled growth eventually leads to the formation of a tumour, which can invade surrounding tissues and, in some cases, spread to other parts of the body through a process called metastasis.
Main Causes of Cancer
- Genetic Mutations
Cancer often arises due to genetic mutations, which can be inherited or acquired over a person’s lifetime. Inherited mutations, like those in the BRCA1 and BRCA2 genes, increase the risk of certain cancers, while acquired mutations can result from various environmental and lifestyle factors.
- Lifestyle Factors
Unhealthy lifestyle choices significantly contribute to cancer risk. Smoking is a leading cause, particularly for lung cancer. Diet and obesity are linked to cancers such as colorectal and breast cancer, while excessive alcohol consumption and lack of physical activity also increase the risk of various cancers.
- Environmental Exposure
Exposure to carcinogens, such as asbestos or certain chemicals, increases cancer risk. Radiation, both from the sun (ultraviolet radiation) and medical imaging (ionizing radiation), can also cause cancer, with skin cancer being a notable example from UV exposure.
- Infections
Certain infections, particularly viral ones, are known to cause cancer. Human papillomavirus (HPV) can lead to cervical and other cancers, while hepatitis B and C are major causes of liver cancer. Chronic bacterial infections like Helicobacter pylori are linked to stomach cancer.
- Immune System Dysfunction
A weakened immune system, whether due to conditions like HIV/AIDS or immunosuppressive medications, increases the risk of developing cancers such as lymphoma and skin cancer. The immune system’s ability to detect and destroy cancer cells is compromised, leading to higher cancer susceptibility.
Treatment of Cancer
Cancer treatment involves various strategies designed to eliminate cancer cells, slow their growth, or manage symptoms. The choice of treatment depends on factors like the type of cancer, its stage, and the patient’s overall health. Common treatment options include surgery, radiation therapy, chemotherapy, targeted therapy, immunotherapy, hormone therapy, stem cell transplants, and palliative care, each offering different benefits depending on the specific circumstances of the patient.
- Surgery
Surgery is a common treatment for cancer, especially when the disease is localized and can be physically removed. The goal of surgery is to excise the tumour along with some surrounding healthy tissue to ensure all cancerous cells are removed. Depending on the size, location, and type of cancer, different surgical techniques may be employed. For instance, minimally invasive surgery, such as laparoscopic or robotic surgery, can be used for smaller tumours and typically involves smaller incisions, leading to quicker recovery times. In contrast, more extensive surgeries, such as a mastectomy for breast cancer, may be necessary for larger or more advanced tumours. Surgery may also be used in combination with other treatments like chemotherapy or radiation therapy to improve outcomes.
- Radiation Therapy
Radiation therapy uses high-energy radiation to target and kill cancer cells by damaging their DNA, thereby preventing them from growing and dividing. This treatment can be used as a primary method to shrink tumours or in conjunction with surgery to eliminate any remaining cancer cells. External beam radiation is the most common form, where a machine directs radiation at the cancer from outside the body. Another method, brachytherapy, involves placing radioactive material inside the body near the tumour, providing a higher dose of radiation to a more localized area. Radiation therapy is particularly useful for treating cancers that are difficult to operate on, such as those located in the brain, or for managing symptoms in advanced cancer cases.

- Chemotherapy
Chemotherapy involves the use of powerful drugs to kill rapidly dividing cancer cells. It is a systemic treatment, meaning the drugs circulate throughout the body, making it effective for treating cancers that have spread, or metastasized, to other parts of the body. Chemotherapy can be administered before surgery to shrink tumours, making them easier to remove, or after surgery to kill any remaining cancer cells. However, because chemotherapy also affects healthy rapidly dividing cells, such as those in the bone marrow, hair follicles, and digestive tract, it can cause significant side effects, including fatigue, nausea, hair loss, and an increased risk of infection. Despite these side effects, chemotherapy remains a cornerstone of cancer treatment.
- Targeted Therapy
Targeted therapy represents a more precise approach to cancer treatment by focusing on specific molecular changes that drive the growth and spread of cancer. Unlike traditional chemotherapy, which can affect both cancerous and healthy cells, targeted therapy specifically aims at the cancer cells, reducing the likelihood of damaging healthy cells. For example, monoclonal antibodies are designed to recognize and bind to specific proteins on the surface of cancer cells, blocking their growth signals. Similarly, small-molecule inhibitors can block the action of enzymes or other proteins involved in cancer cell proliferation. Targeted therapies are often used in cancers that have specific genetic mutations or protein expressions, such as HER2-positive breast cancer or certain types of leukaemia.
- Immunotherapy
Immunotherapy is a treatment that harnesses the power of the body’s immune system to fight cancer. This approach is particularly effective in certain cancers, such as melanoma and lung cancer, where the immune system can be stimulated to recognize and destroy cancer cells. One type of immunotherapy, immune checkpoint inhibitors, works by blocking proteins that prevent immune cells from attacking cancer cells, thereby enhancing the immune response. Another form, CAR T-cell therapy, involves modifying a patient’s T-cells (a type of immune cell) in a laboratory to better target and kill cancer cells. Additionally, cancer vaccines and other immunotherapies are being developed to further boost the immune system’s ability to combat cancer. Immunotherapy can lead to durable responses and, in some cases, long-term remission.
- Hormone Therapy
Hormone therapy is used to treat cancers that rely on hormones to grow, such as breast and prostate cancers. This treatment works by either lowering the levels of hormones in the body or by blocking their effects on cancer cells. For example, in estrogen-receptor-positive breast cancer, drugs like tamoxifen or aromatase inhibitors can be used to block estrogen’s ability to stimulate cancer growth. In prostate cancer, androgen deprivation therapy reduces levels of male hormones that can fuel cancer growth. Hormone therapy can be used alone or in combination with other treatments, such as surgery or radiation therapy, and is often part of long-term treatment plans to reduce the risk of cancer recurrence.
- Stem Cell Transplant
Stem cell transplants, also known as bone marrow transplants, are used to restore healthy stem cells in patients whose bone marrow has been damaged or destroyed by high-dose chemotherapy or radiation therapy. This treatment is commonly used for blood-related cancers like leukaemia, lymphoma, and multiple myeloma. There are two main types of stem cell transplants: autologous transplants, which use the patient’s own stem cells, and allogeneic transplants, which use stem cells from a donor. The transplanted stem cells help regenerate the patient’s bone marrow, allowing the body to produce healthy blood cells. While stem cell transplants can be life-saving, they also carry significant risks, including infections and graft-versus-host disease, where the donor cells attack the patient’s tissues.
- Palliative Care
Palliative care is a specialized approach focused on providing relief from the symptoms, pain, and stress of cancer, especially in advanced stages. The goal of palliative care is to improve the quality of life for both the patient and their family, regardless of the stage of the disease or the type of treatment being received. It can include pain management, emotional support, and assistance with decision-making regarding treatment options. Palliative care can be provided alongside curative treatments to help manage side effects, or it may become the primary focus of care when the cancer is no longer responding to treatment. By addressing the physical, emotional, and psychological needs of the patient, palliative care plays a crucial role in comprehensive cancer care.
Cancer Prevention
- Avoid Tobacco: Refrain from smoking and avoid second hand smoke to lower the risk of lung and other cancers.
- Healthy Diet: Eat a balanced diet rich in fruits, vegetables, and whole grains; limit processed foods and red meat.
- Regular Exercise: Stay active to maintain a healthy weight and reduce the risk of cancers like breast and colon cancer.
- Limit Alcohol: Reduce alcohol intake to lower the risk of breast, liver, and esophageal cancers.
- Sun Protection: Use sunscreen and avoid excessive sun exposure to prevent skin cancer.
- Vaccinations: Get vaccinated against HPV and hepatitis B to reduce the risk of cervical and liver cancers.
- Health Screenings: Participate in regular screenings (e.g., mammograms, colonoscopies) for early detection and prevention.
- Limit Carcinogen Exposure: Minimize exposure to harmful chemicals and radiation.
- Maintain Healthy Weight: Manage weight through diet and exercise to reduce the risk of various cancers.
Conclusion
Cancer remains one of the most significant health challenges worldwide, affecting millions of people each year. Through this investigatory project, we have explored the fundamental aspects of cancer, including its definition, types, causes, symptoms, and the differences between normal and cancerous cells. We also examined the various treatments available and emphasized the importance of early detection and prevention strategies.
Understanding cancer at a cellular level reveals the complexity of this disease and underscores the need for ongoing research and education. The project has highlighted how lifestyle choices, genetic factors, and environmental exposures contribute to the development of cancer, making prevention efforts crucial in reducing the incidence of this disease.